A comprehensive new report compiled by researchers at the Food is Medicine Institute at Tufts University has quantified the potential health and economic benefits of Food is Medicine (FIM) — food-based nutritional interventions that aim to treat or prevent disease.
While poor nutrition and food insecurity are major drivers of poor health outcomes and excess healthcare spending in the U.S., few strategies or programs within the healthcare system exist to address these risks.
“It is time to recognize the true cost of food and take action as a country by placing a stronger emphasis on providing healthy food as a tool for treating chronic disease,” said Dariush Mozaffarian, MD, Director at Food is Medicine Institute, in the report.
The Burdens of Poor Nutrition
When it comes to consuming a healthy diet, most Americans have a suboptimal score.
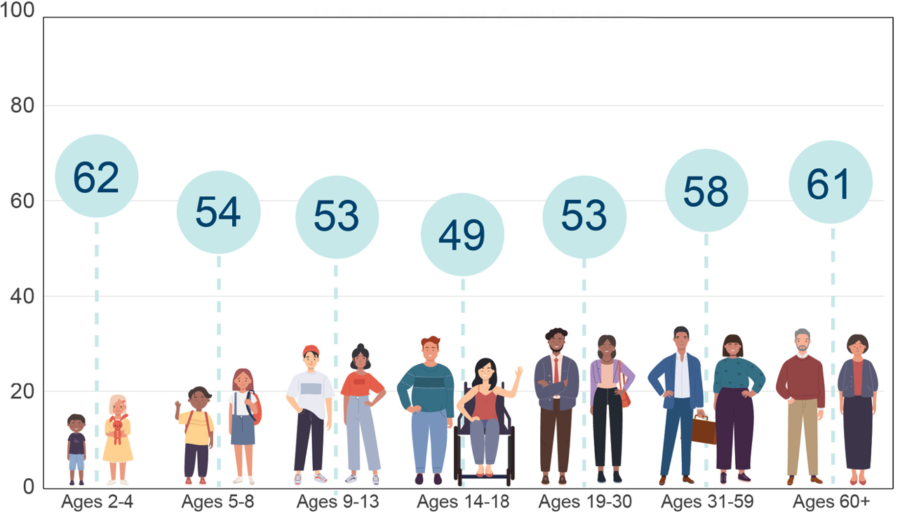
Source: U.S. Department of Agriculture Food and Nutrition Service. How Healthy is the American Diet? Published October 2021.
Across the population, the average Healthy Eating Index (HEI) score — a measure of diet quality that assesses alignment with the Dietary Guidelines for Americans — is 58 out of 100.
Poor nutrition is the leading driver of death and disability in the U.S., including from heart disease, stroke, type 2 diabetes, obesity, hypertension, and some cancers.
The costs of suboptimal diets due to health care spending and lost productivity are estimated at $1.1 trillion each year — equaling the economic output of the entire food sector.
To better understand the potential national impacts of key FIM strategies, Tufts University conducted two separate case studies to gauge the national impact of scaling medically tailored meals (MTMs) and produce prescription programs.
Medically Tailored Meals
In the first case study, eligible patients received 10 weekly meals that were medically tailored by Registered Dietitian Nutritionists, for an average of 8 months each year.
Key findings:
- Among 6.3 million eligible recipients, provision of MTMs could lead to 6 million fewer hospitalizations annually.
- The policy was anticipated to reduce healthcare system costs with estimated net savings of $13.6 billion over one year and $185.1 billion over 10 years.
- By payer subsets, one-year possible policy cost savings were estimated at $3.0 billion for private payers ($476 per), $3.3 billion for Medicare ($523 per), $1.6 billion for Medicaid ($253 per), and $5.7 billion for dual-eligible individuals ($904 per couple).
Produce Prescription Programs
In the second case study, eligible patients received food boxes or prepaid vouchers with an average monthly allotment of $42 per patient or $504/year to purchase fruits and vegetables from major retail locations.
Key findings:
- Among 6.5 million eligible recipients, provision of produce prescriptions over a lifetime would prevent 292,000 cardiovascular disease (CVD) events and generate 260,000 quality-adjusted life-years (QALYs).
- There was an estimated $44.3 billion in programs costs and an estimated savings of $39.6 billion in healthcare costs and $4.77 billion in productivity costs over a lifetime.
- Compared to modern weight loss medications, produce prescriptions are much more cost effective. The estimated incremental cost-effective ratio for weight loss medications is about $200,000/ QALY, which equates to more than ten times higher cost per health gained than produce prescriptions.
“These two case studies of suggest that Food is Medicine interventions scaled to a national level in the U.S. would not only improve health and be highly cost effective, but also serve as a cost saving intervention in the healthcare setting for addressing diet-related chronic illness and health inequities,” the research team observed in the report. “This is a rare outcome in medical care as few — if any — other interventions in healthcare are both cost effective and cost saving.”












